Lyme disease is the most common tick-borne disease in British Columbia (BC) and North America. It is transmitted by the bite of Ixodes ticks. These ticks are distributed throughout BC, but they are most commonly found in southwestern BC, including Vancouver Island, the Gulf Islands, the Sunshine Coast, Greater Vancouver, and the Fraser Valley. The geographic distribution of Lyme disease in people and in ticks in BC has remained constant over time. In BC, from 2013–2022, 6–39 cases of Lyme disease were reported each year; most are related to out-of-province travel. Locally acquired cases range from 1 – 14 cases per year.
In BC, less than 1 percent of ticks tested carry the bacteria
B. burgdorferi that cause Lyme disease. For more details on tick surveillance in BC, see the BCCDC’s
surveillance report. Although the number of ticks submitted for testing has increased in recent years, the prevalence of
B. burgdorferi in ticks has remained consistently
low over time.
The risk of Lyme disease in BC is lower and more stable than it is in eastern and central Canada and in the northeastern USA. Reasons for this difference include:
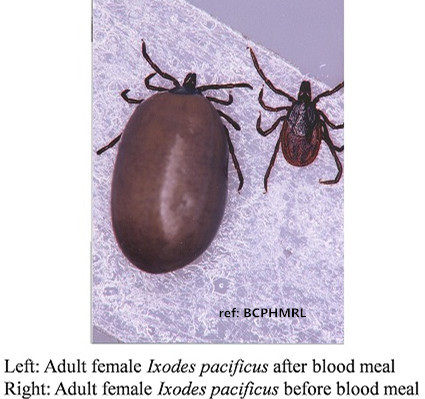
- The tick species capable of carrying Lyme disease in BC are different. I. pacificus (western black-legged ticks) and I. angustus are less capable of transmitting B. burgdorferi than I. scapularis (blacklegged tick), a tick found in eastern Canada.
- The animals on which these ticks feed are different. In BC, ticks feed on small rodents such as deer mice and dusky-footed woodrats, and lizards such as the Northern alligator lizard that may contain an anti-bacterial property. In eastern Canada and the USA, ticks feed on white-footed mice and white-tailed deer.
- The vegetation and climate are different between BC and eastern Canada (e.g. BC has mostly coniferous forests, whereas eastern Canada has mostly leafy forests).
Lyme disease is caused by a bacterium called Borrelia burgdorferi that is spread by ticks. B. burgdorferi has been found in two species of ticks in BC: Ixodes pacificus also known as western black-legged tick, and Ixodes angustus.
If you have the following symptoms within 3-30 days after being bitten by a tick or after having been in tall grassy or wooded areas known to have Lyme disease, consult your healthcare provider. Tell your doctor when and where you were bitten by a tick.
- Skin rash: About 70-80% of patients have a skin rash at the site of the tick bite. The rash feels warm but is not itchy or painful. It expands over a few days and can reach up to 30 cm across. Parts of the rash may clear as it enlarges, resulting in a “bull's-eye” appearance. This is called erythema migrans. Some people may not experience a rash.

- Fever
- Headache
- Muscle and joint pains
- Fatigue
Illness can progress over weeks and months and cause more bull’s-eye rashes, inflammation of the heart leading to impaired electrical conduction, as well as neurological symptoms. These symptoms include inflammation of the lining around the brain and the spinal cord, nerve pain and dysfunction, and weakness or paralysis of the muscles of the face.
Although less common people with Lyme disease who were not treated may develop joint and neurological complications months or years later. About 60% of untreated patients have bouts of arthritis, with severe joint pain and swelling. Large joints are most often affected, particularly the knees. In rare cases, untreated patients develop chronic neurological complaints. These include shooting pains, numbness or tingling in the hands or feet, and problems with short-term memory.
About 10-20% of patients with Lyme disease have symptoms that last months to years after treatment with antibiotics. These symptoms can include muscle and joint pains, cognitive defects, sleep disturbance, or fatigue. The cause of these symptoms is not known, but there is no evidence that these symptoms are due to ongoing infection with B. burgdorferi.
If you have symptoms such as fatigue, pain, poor sleep and problems with brain function and test negative for Lyme disease, or persistent symptoms after treatment for Lyme disease, please consult the BC Women's Hospital Complex Chronic Disease Program for further support.
Lyme disease is diagnosed based on symptoms, a physical exam, the possibility of exposure to infected ticks and laboratory testing. If your healthcare provider suspects Lyme disease, you may be asked to provide a blood sample for testing. Laboratory testing is not recommended for patients who do not have symptoms consistent with Lyme disease.
Laboratory tests support clinical care when used correctly and are performed using validated methods in an accredited laboratory. In BC, laboratory testing to diagnose Lyme disease is done by the
BCCDC Public Health Laboratory (PHL), a laboratory accredited by the College of American Pathologists and the Diagnostic Accreditation Program. BCCDC PHL follows the US Centers for Disease Control & Prevention and Public Health Agency of Canada recommended process to assess for evidence of antibodies against the Lyme disease bacteria.
Blood tests may not be positive in early infection. Therefore:
- Symptoms of early Lyme disease (e.g. rash) following tick exposure may be treated by your healthcare provider on clinical grounds, even without a positive test.
- Repeat testing a few months after an initial negative test may be warranted if there are ongoing symptoms.
In BC, less than 1% of the ticks submitted to BCCDC carry Borrelia borgdorferi (bacteria that causes Lyme Disease), so antibiotic prophylaxis (medicine given as prevention in the absence of symptoms) is usually not necessary after a bite from a BC tick. For tick bites that occur outside of BC, your health care provider may recommend prophylaxis based on many factors, including the tick species involved, how commonly that tick carries the disease in that area, how long it was on the body, and whether there are more benefits or possible harms from antibiotic use for you.
If Lyme disease is confirmed or strongly suspected based on tick exposure and symptoms, early treatment is recommended.
Certain animals, like dogs, horses, and cows, can also get Lyme disease with symptoms similar to those seen in humans. Dogs are particularly susceptible. Symptoms may not appear for 7-21 days or longer after a tick bite, so watch your dog closely for changes in behaviour or appetite. Tick bites on dogs may be hard to detect. If you find a tick on your dog, remove it as you would in a human.
To reduce the chances that a tick will transmit disease to your pets:
- Check your pets for ticks after they spend time outdoors.
- If you find a tick on your dog, remove it right away.
- Ask your veterinarian to conduct a tick check at each exam.
- Talk to your veterinarian about tick-borne diseases in your area.
- Talk with your veterinarian about using tick preventives on your pet.
